Member Stories
You are not alone. Read the roads taken by others.
My journey with prostate cancer started about 12 years ago with a phone call from my father. At age 75 he had been diagnosed with metastasis prostate cancer. I had just turned 50. My knowledge of prostate cancer was very limited. I called our family doctor who filled me in with information about what to expect with my father and also suggested that I start regular psa testing. I soon started getting regular dre's and psa tests. My father went on to hormonal therapy and lived another 4 years, ultimately dying of a heart attack.
During this period every time I went for a test I heard "everything's normal". When I was 55 my psa came back at 3.6 and I was sent to an urologist. Again, "everything's normal - come back next year." The following year my psa climbed to 5.6 and a subsequent biopsy gave me a Gleason score of 6, and six positive core samples out of 6 taken. I had prostate cancer!
My urologist told me that surgery was my best option, but because of the extent of the cancer and the good possibility of it having spread outside the capsule, he would have to be aggressive in his surgery. He assured me I would most likely be impotent, and possibly suffer from incontinence. Radiation was also mentioned as a secondary treatment if the surgery failed. Needless to say I was in shock! I was 56 and I had thought, healthy. My routine for over 8 years was to swim a mile a day, watch what I eat and drink and not smoke. I had no symptoms and felt great. But suddenly I felt like my life was over.
After getting over the initial shock I decided to be equally aggressive in my search for treatment options. I went first to the library. Remember, this was almost six years ago. The books I found were not very helpful. Most dealt with surgery – the operation, recovery, living with side effects, etc. While I was doing research I sent copies of my biopsy slides to Memorial Sloan Kettering Hospital in New York for a second opinion. I also sought out and had an appointment with another urologist in another city. The internet provided me with links to other treatments, to survivors, and prostate cancer specialists. To make a long story short I finally linked up with Dr. Haakon Ragde in Seattle, Washington. His recommendation was three-fold. A 4 month course of hormones (Zoladex and Flutamide), 25 sessions of external beam radiation and finally brachytherapy – the insertion of tiny radioactive seeds directly into the prostate gland under ultrasound guidance.
I went with his recommendations. The hormonal therapy and external beam radiation was provided by the caring staff at Tom Baker Cancer Centre in Calgary. As brachy was not yet available in Canada I had that procedure done in Seattle. I finished my treatment in December, 1997.
Now over seven years out and my psa is stable at 0.1. My quality of life is excellent. Knowing what I know now, would I do it again? Absolutely. But I also recognize that my choice of treatment, while right for me, is not necessarily right for others.
Since my diagnosis I have become very active in the prostate cancer support community. I took over as President of PCCN Calgary (the local support group) 4 years ago and in January 2003 became President of the Prostate Cancer Canada Network.
Prostate Cancer support groups fulfill an important role. They are there when the newly diagnosed need someone to talk too right now! They can also provide up-to-date information on various treatment modalities. Many groups regularly feature medical guest speakers at monthly meetings to keep members informed. Building awareness for early detection and advocating for treatment options are also important functions of the groups.
PCCN Calgary's mission statement says it all: "Our objective is to assist and support patients, families and friends as they deal with prostate cancer. We inform, empathize and reassure men on their journey. We share our experiences with our own cancer, lift our spirits and strengthen our resolve to fight for quality of life and a cure."
PCCN is the national organization representing some 120 independent support groups across the country. PCCN speaks for tens of thousands of men suffering from prostate cancer to government and business. PCCN builds awareness through projects like "Living Proof" – a national awareness campaign featuring prostate cancer survivors and a soon to be released national television campaign featuring Red Green.
What can be done to help in the battle with prostate cancer? If you're a man over 50 or over 40 with a family history of cancer, talk to your doctor about getting tested. Watch your diet and exercise regularly. If you have already been diagnosed, get in touch with your local support group. Our web site at www.prostatecancer.ca. is a good source of links and information about prostate cancer and provides contact information to groups across the country.
One in three Canadians will experience cancer. In my family, my father had prostate cancer, my mother died with ovarian cancer, and my wife was diagnosed and successfully treated for breast cancer 6 months after my initial prostate cancer diagnosis. Having faced cancer, and at least for the time being having beaten it, I now have a much greater appreciation for each day. I firmly believe that maintaining a positive attitude and helping others along their journey goes a long way to a successful recovery.
During this period every time I went for a test I heard "everything's normal". When I was 55 my psa came back at 3.6 and I was sent to an urologist. Again, "everything's normal - come back next year." The following year my psa climbed to 5.6 and a subsequent biopsy gave me a Gleason score of 6, and six positive core samples out of 6 taken. I had prostate cancer!
My urologist told me that surgery was my best option, but because of the extent of the cancer and the good possibility of it having spread outside the capsule, he would have to be aggressive in his surgery. He assured me I would most likely be impotent, and possibly suffer from incontinence. Radiation was also mentioned as a secondary treatment if the surgery failed. Needless to say I was in shock! I was 56 and I had thought, healthy. My routine for over 8 years was to swim a mile a day, watch what I eat and drink and not smoke. I had no symptoms and felt great. But suddenly I felt like my life was over.
After getting over the initial shock I decided to be equally aggressive in my search for treatment options. I went first to the library. Remember, this was almost six years ago. The books I found were not very helpful. Most dealt with surgery – the operation, recovery, living with side effects, etc. While I was doing research I sent copies of my biopsy slides to Memorial Sloan Kettering Hospital in New York for a second opinion. I also sought out and had an appointment with another urologist in another city. The internet provided me with links to other treatments, to survivors, and prostate cancer specialists. To make a long story short I finally linked up with Dr. Haakon Ragde in Seattle, Washington. His recommendation was three-fold. A 4 month course of hormones (Zoladex and Flutamide), 25 sessions of external beam radiation and finally brachytherapy – the insertion of tiny radioactive seeds directly into the prostate gland under ultrasound guidance.
I went with his recommendations. The hormonal therapy and external beam radiation was provided by the caring staff at Tom Baker Cancer Centre in Calgary. As brachy was not yet available in Canada I had that procedure done in Seattle. I finished my treatment in December, 1997.
Now over seven years out and my psa is stable at 0.1. My quality of life is excellent. Knowing what I know now, would I do it again? Absolutely. But I also recognize that my choice of treatment, while right for me, is not necessarily right for others.
Since my diagnosis I have become very active in the prostate cancer support community. I took over as President of PCCN Calgary (the local support group) 4 years ago and in January 2003 became President of the Prostate Cancer Canada Network.
Prostate Cancer support groups fulfill an important role. They are there when the newly diagnosed need someone to talk too right now! They can also provide up-to-date information on various treatment modalities. Many groups regularly feature medical guest speakers at monthly meetings to keep members informed. Building awareness for early detection and advocating for treatment options are also important functions of the groups.
PCCN Calgary's mission statement says it all: "Our objective is to assist and support patients, families and friends as they deal with prostate cancer. We inform, empathize and reassure men on their journey. We share our experiences with our own cancer, lift our spirits and strengthen our resolve to fight for quality of life and a cure."
PCCN is the national organization representing some 120 independent support groups across the country. PCCN speaks for tens of thousands of men suffering from prostate cancer to government and business. PCCN builds awareness through projects like "Living Proof" – a national awareness campaign featuring prostate cancer survivors and a soon to be released national television campaign featuring Red Green.
What can be done to help in the battle with prostate cancer? If you're a man over 50 or over 40 with a family history of cancer, talk to your doctor about getting tested. Watch your diet and exercise regularly. If you have already been diagnosed, get in touch with your local support group. Our web site at www.prostatecancer.ca. is a good source of links and information about prostate cancer and provides contact information to groups across the country.
One in three Canadians will experience cancer. In my family, my father had prostate cancer, my mother died with ovarian cancer, and my wife was diagnosed and successfully treated for breast cancer 6 months after my initial prostate cancer diagnosis. Having faced cancer, and at least for the time being having beaten it, I now have a much greater appreciation for each day. I firmly believe that maintaining a positive attitude and helping others along their journey goes a long way to a successful recovery.

Bob Shiell
Prostaid Founder
My journey with prostate cancer started about 12 years ago with a phone call from my father. At age 75 he had been diagnosed with metastasis prostate cancer. I had just turned 50. My knowledge of prostate cancer was very limited. I called our family doctor who filled me in with information about what to expect with my father and also suggested that I start regular psa testing. I soon started getting regular dre's and psa tests. My father went on to hormonal therapy and lived another 4 years, ultimately dying of a heart attack.
During this period every time I went for a test I heard "everything's normal". When I was 55 my psa came back at 3.6 and I was sent to an urologist. Again, "everything's normal - come back next year." The following year my psa climbed to 5.6 and a subsequent biopsy gave me a Gleason score of 6, and six positive core samples out of 6 taken. I had prostate cancer!
My urologist told me that surgery was my best option, but because of the extent of the cancer and the good possibility of it having spread outside the capsule, he would have to be aggressive in his surgery. He assured me I would most likely be impotent, and possibly suffer from incontinence. Radiation was also mentioned as a secondary treatment if the surgery failed. Needless to say I was in shock! I was 56 and I had thought, healthy. My routine for over 8 years was to swim a mile a day, watch what I eat and drink and not smoke. I had no symptoms and felt great. But suddenly I felt like my life was over.
After getting over the initial shock I decided to be equally aggressive in my search for treatment options. I went first to the library. Remember, this was almost six years ago. The books I found were not very helpful. Most dealt with surgery – the operation, recovery, living with side effects, etc. While I was doing research I sent copies of my biopsy slides to Memorial Sloan Kettering Hospital in New York for a second opinion. I also sought out and had an appointment with another urologist in another city. The internet provided me with links to other treatments, to survivors, and prostate cancer specialists. To make a long story short I finally linked up with Dr. Haakon Ragde in Seattle, Washington. His recommendation was three-fold. A 4 month course of hormones (Zoladex and Flutamide), 25 sessions of external beam radiation and finally brachytherapy – the insertion of tiny radioactive seeds directly into the prostate gland under ultrasound guidance.
I went with his recommendations. The hormonal therapy and external beam radiation was provided by the caring staff at Tom Baker Cancer Centre in Calgary. As brachy was not yet available in Canada I had that procedure done in Seattle. I finished my treatment in December, 1997.
Now over seven years out and my psa is stable at 0.1. My quality of life is excellent. Knowing what I know now, would I do it again? Absolutely. But I also recognize that my choice of treatment, while right for me, is not necessarily right for others.
Since my diagnosis I have become very active in the prostate cancer support community. I took over as President of PCCN Calgary (the local support group) 4 years ago and in January 2003 became President of the Prostate Cancer Canada Network.
Prostate Cancer support groups fulfill an important role. They are there when the newly diagnosed need someone to talk too right now! They can also provide up-to-date information on various treatment modalities. Many groups regularly feature medical guest speakers at monthly meetings to keep members informed. Building awareness for early detection and advocating for treatment options are also important functions of the groups.
PCCN Calgary's mission statement says it all: "Our objective is to assist and support patients, families and friends as they deal with prostate cancer. We inform, empathize and reassure men on their journey. We share our experiences with our own cancer, lift our spirits and strengthen our resolve to fight for quality of life and a cure."
PCCN is the national organization representing some 120 independent support groups across the country. PCCN speaks for tens of thousands of men suffering from prostate cancer to government and business. PCCN builds awareness through projects like "Living Proof" – a national awareness campaign featuring prostate cancer survivors and a soon to be released national television campaign featuring Red Green.
What can be done to help in the battle with prostate cancer? If you're a man over 50 or over 40 with a family history of cancer, talk to your doctor about getting tested. Watch your diet and exercise regularly. If you have already been diagnosed, get in touch with your local support group. Our web site at www.prostatecancer.ca. is a good source of links and information about prostate cancer and provides contact information to groups across the country.
One in three Canadians will experience cancer. In my family, my father had prostate cancer, my mother died with ovarian cancer, and my wife was diagnosed and successfully treated for breast cancer 6 months after my initial prostate cancer diagnosis. Having faced cancer, and at least for the time being having beaten it, I now have a much greater appreciation for each day. I firmly believe that maintaining a positive attitude and helping others along their journey goes a long way to a successful recovery.
During this period every time I went for a test I heard "everything's normal". When I was 55 my psa came back at 3.6 and I was sent to an urologist. Again, "everything's normal - come back next year." The following year my psa climbed to 5.6 and a subsequent biopsy gave me a Gleason score of 6, and six positive core samples out of 6 taken. I had prostate cancer!
My urologist told me that surgery was my best option, but because of the extent of the cancer and the good possibility of it having spread outside the capsule, he would have to be aggressive in his surgery. He assured me I would most likely be impotent, and possibly suffer from incontinence. Radiation was also mentioned as a secondary treatment if the surgery failed. Needless to say I was in shock! I was 56 and I had thought, healthy. My routine for over 8 years was to swim a mile a day, watch what I eat and drink and not smoke. I had no symptoms and felt great. But suddenly I felt like my life was over.
After getting over the initial shock I decided to be equally aggressive in my search for treatment options. I went first to the library. Remember, this was almost six years ago. The books I found were not very helpful. Most dealt with surgery – the operation, recovery, living with side effects, etc. While I was doing research I sent copies of my biopsy slides to Memorial Sloan Kettering Hospital in New York for a second opinion. I also sought out and had an appointment with another urologist in another city. The internet provided me with links to other treatments, to survivors, and prostate cancer specialists. To make a long story short I finally linked up with Dr. Haakon Ragde in Seattle, Washington. His recommendation was three-fold. A 4 month course of hormones (Zoladex and Flutamide), 25 sessions of external beam radiation and finally brachytherapy – the insertion of tiny radioactive seeds directly into the prostate gland under ultrasound guidance.
I went with his recommendations. The hormonal therapy and external beam radiation was provided by the caring staff at Tom Baker Cancer Centre in Calgary. As brachy was not yet available in Canada I had that procedure done in Seattle. I finished my treatment in December, 1997.
Now over seven years out and my psa is stable at 0.1. My quality of life is excellent. Knowing what I know now, would I do it again? Absolutely. But I also recognize that my choice of treatment, while right for me, is not necessarily right for others.
Since my diagnosis I have become very active in the prostate cancer support community. I took over as President of PCCN Calgary (the local support group) 4 years ago and in January 2003 became President of the Prostate Cancer Canada Network.
Prostate Cancer support groups fulfill an important role. They are there when the newly diagnosed need someone to talk too right now! They can also provide up-to-date information on various treatment modalities. Many groups regularly feature medical guest speakers at monthly meetings to keep members informed. Building awareness for early detection and advocating for treatment options are also important functions of the groups.
PCCN Calgary's mission statement says it all: "Our objective is to assist and support patients, families and friends as they deal with prostate cancer. We inform, empathize and reassure men on their journey. We share our experiences with our own cancer, lift our spirits and strengthen our resolve to fight for quality of life and a cure."
PCCN is the national organization representing some 120 independent support groups across the country. PCCN speaks for tens of thousands of men suffering from prostate cancer to government and business. PCCN builds awareness through projects like "Living Proof" – a national awareness campaign featuring prostate cancer survivors and a soon to be released national television campaign featuring Red Green.
What can be done to help in the battle with prostate cancer? If you're a man over 50 or over 40 with a family history of cancer, talk to your doctor about getting tested. Watch your diet and exercise regularly. If you have already been diagnosed, get in touch with your local support group. Our web site at www.prostatecancer.ca. is a good source of links and information about prostate cancer and provides contact information to groups across the country.
One in three Canadians will experience cancer. In my family, my father had prostate cancer, my mother died with ovarian cancer, and my wife was diagnosed and successfully treated for breast cancer 6 months after my initial prostate cancer diagnosis. Having faced cancer, and at least for the time being having beaten it, I now have a much greater appreciation for each day. I firmly believe that maintaining a positive attitude and helping others along their journey goes a long way to a successful recovery.

Bob Shiell
Prostaid Founder
In 2003 at age 63, my PSA had gone up to 5.7 from 3.9 in 2001 so off to the urologist for a biopsy. Results in Nov 2003 were positive, Gleason 3+3=6 which is not too alarming (they say). After some research we decided on a prostatectomy which was booked for Feb 2004. Cryotherapy was not being funded by Alberta Health Care at that time. In Jan 2004 I had a heart attack! The cardiologist's fixed me up with an angioplasty & a bunch of pills but the urologist postponed the prostatectomy for 6 months to July 2004! In March 2004 another heart vessel decided to shut off so back to the cardio's for another angioplasty and 3 months of lectures & exercises at the Cardiac Wellness Centre at Lindsay Park. We try to follow Dr. Dean Ornish's Program for Reversing Heart Disease (primarily less than 25 grams of fat per day). The bad news was that the urologist cancelled the prostatectomy, too much trauma for someone with 2 heart attacks!
So back to the alternative treatments. My GP had a patient who had had cryo in Ontario and was doing very well and, fortunately by this time, Dr Donnelly was doing it in Calgary and AHC had approved funding. So the old CaP was culled by icing in Sep 2004 with 1 night in hospital and very little suffering. We are (so far) living happily ever after with PSA at 0. The only casualty is sex life but "been there, done that" so after 43 years of marriage it's not a big deal anymore. Thankfully the heart has been working good for the last 2.5 years.
So back to the alternative treatments. My GP had a patient who had had cryo in Ontario and was doing very well and, fortunately by this time, Dr Donnelly was doing it in Calgary and AHC had approved funding. So the old CaP was culled by icing in Sep 2004 with 1 night in hospital and very little suffering. We are (so far) living happily ever after with PSA at 0. The only casualty is sex life but "been there, done that" so after 43 years of marriage it's not a big deal anymore. Thankfully the heart has been working good for the last 2.5 years.

Marvin Crowley
Starting at about age 50 ( I am 73 years young now ) I requested a PSA Test with my annual exam. The PSA test showed counts between 2.5 and 3.5 over many years.
Then in 2001, during my annual exam, I was told that my PSA count had gone up to 3.9.
My Doctor ( at that time on Pender Island B.C where we moved when I retired in 1992 ) suggested another test a few months later. The next test came in at 4.3.
The Doctor sent me to a Urologist in Victoria who arranged for me to have a biopsy. The biopsy showed that I did, in fact, have Prostate Cancer.¬¬ Not a good day.
I met with an Oncologist in Victoria , who went over the options with me. I decided on a Radical Prostatectomy , as I was otherwise very healthy...... and had the operation in Victoria in 2001.
The operation went very smoothly and I felt quite well after the operation and from that time on. ( I never did feel too excited about the catheter, but found it quite handy if I got caught short while out on a long walk ) I was told by the Oncologist that the cancer in the prostate came right out to the edge of the prostate and that he took out some extra tissue around the prostate. He was hopeful ( as were we ) that he got it all.
Well, my PSA count for the next five years came in at 0.1 or less and to say the least, I was delighted. I was beginning to think I had that nasty cancer beat.
Then in December 2005,during an annual exam ( we moved back to Calgary after the operation in 2001 ), we learned that the cancer had returned. My count came in at 2.5.
I met with my Urologist and Oncologist and after considerable discussion about the various options, I decided to go for radiation rather than " wait and watch" which was another option.
By the time I went for my first Radiation Treatment in January my count was 3.3 (still quite low in many peoples minds).
I had 36 radiation treatments.....one each week day for 7 weeks. The treatments went very well and I experienced only a few side effects as I progressed through the treatments. About half way through the treatments I started having some bowel problems......having to " go " more often than normal,.....much more often ! A nurse at the Tom Baker Cancer asked me if I took Metamucil and I told her I had been taking it for years. She suggested that I put a HEAPING TEASPOON of Metamucil in a HALF GLASS of water before retiring each night and then continue with my normal dosage during the day. This suggestion worked wonderfully and I, at least , didn't have any problems at night. I had a couple days when I felt nauseated but nothing that kept us from being out and about every day. I did not lose a pound during radiation. (maybe it was because we stopped somewhere for a treat after each treatment!).
I was very happy with my Urologist, Oncologist and the folks at the Tom Baker Cancer Center. I was particularly impressed with a lovely lady on the reception desk at the Cancer Center. I called her " Sparkle" because she had a special talent making people smile. I also became very fond of the wonderful ladies who got me set up for each treatment. What a beautiful group of ladies. They had a special way of making you feel that every thing would be OK.
My last radiation treatment was on Mar 6th 2006 and my Oncologist explained that I would not get the results of the radiation for 6 months.
On September 6th 2006 , I went to the office of my Oncologist at Tom Baker Center and he gave me the results of the PSA test I had 2 weeks earlier.
I should tell you, that for a considerable time before this appointment, I was a very concerned man. (I should say I am a born worrier). A lot of different thoughts were going through my head.
My Oncologist explained that my PSA Test came in at 0.03 (compared to 0.33 at the beginning of the treatments).
To say the least my wife and I were very thankful.
My next PSA Test will be in February 2007, and we hope and pray that the news will be encouraging again.
We have much to be thankful for.
Then in 2001, during my annual exam, I was told that my PSA count had gone up to 3.9.
My Doctor ( at that time on Pender Island B.C where we moved when I retired in 1992 ) suggested another test a few months later. The next test came in at 4.3.
The Doctor sent me to a Urologist in Victoria who arranged for me to have a biopsy. The biopsy showed that I did, in fact, have Prostate Cancer.¬¬ Not a good day.
I met with an Oncologist in Victoria , who went over the options with me. I decided on a Radical Prostatectomy , as I was otherwise very healthy...... and had the operation in Victoria in 2001.
The operation went very smoothly and I felt quite well after the operation and from that time on. ( I never did feel too excited about the catheter, but found it quite handy if I got caught short while out on a long walk ) I was told by the Oncologist that the cancer in the prostate came right out to the edge of the prostate and that he took out some extra tissue around the prostate. He was hopeful ( as were we ) that he got it all.
Well, my PSA count for the next five years came in at 0.1 or less and to say the least, I was delighted. I was beginning to think I had that nasty cancer beat.
Then in December 2005,during an annual exam ( we moved back to Calgary after the operation in 2001 ), we learned that the cancer had returned. My count came in at 2.5.
I met with my Urologist and Oncologist and after considerable discussion about the various options, I decided to go for radiation rather than " wait and watch" which was another option.
By the time I went for my first Radiation Treatment in January my count was 3.3 (still quite low in many peoples minds).
I had 36 radiation treatments.....one each week day for 7 weeks. The treatments went very well and I experienced only a few side effects as I progressed through the treatments. About half way through the treatments I started having some bowel problems......having to " go " more often than normal,.....much more often ! A nurse at the Tom Baker Cancer asked me if I took Metamucil and I told her I had been taking it for years. She suggested that I put a HEAPING TEASPOON of Metamucil in a HALF GLASS of water before retiring each night and then continue with my normal dosage during the day. This suggestion worked wonderfully and I, at least , didn't have any problems at night. I had a couple days when I felt nauseated but nothing that kept us from being out and about every day. I did not lose a pound during radiation. (maybe it was because we stopped somewhere for a treat after each treatment!).
I was very happy with my Urologist, Oncologist and the folks at the Tom Baker Cancer Center. I was particularly impressed with a lovely lady on the reception desk at the Cancer Center. I called her " Sparkle" because she had a special talent making people smile. I also became very fond of the wonderful ladies who got me set up for each treatment. What a beautiful group of ladies. They had a special way of making you feel that every thing would be OK.
My last radiation treatment was on Mar 6th 2006 and my Oncologist explained that I would not get the results of the radiation for 6 months.
On September 6th 2006 , I went to the office of my Oncologist at Tom Baker Center and he gave me the results of the PSA test I had 2 weeks earlier.
I should tell you, that for a considerable time before this appointment, I was a very concerned man. (I should say I am a born worrier). A lot of different thoughts were going through my head.
My Oncologist explained that my PSA Test came in at 0.03 (compared to 0.33 at the beginning of the treatments).
To say the least my wife and I were very thankful.
My next PSA Test will be in February 2007, and we hope and pray that the news will be encouraging again.
We have much to be thankful for.

Don & Nell Jacques
This whole story starts with an annual health check-up with our family doctor in mid-December 1997. About a week later the results indicated that in one of the blood tests suggest that something was amiss in the prostate. A consultation with a urologist was recommended and I concurred immediately. Our family doctor referred me to Dr. Bryan Donnelly. In January 1998 I had my first consultation with him at which time he indicated that there was a likely hood of prostate cancer based on the PSA test. A biopsy revealed a 20% incidence in one of the tissues examined.
What to do next? The doctor explained that there was no hurray, that I would not die because of the "showing". Although my PSA was 7.5 the Gleason score was 2/4 (6). My wife and I decided right there and then I would undergo therapy of some kin. Dr. Donnelly then mentioned he was starting a clinical test program to test the efficacy of cryosurgery, but before any action along this line is undertaken, a series of test would have to be held. After these tests had been completed I was told I was an "excellent candidate" for cryosurgery.
No long after I was contacted by Cheryl Scott RN, the coordinator of the program (incidentally, Cheryl was the one earlier who appraised me of the results of the biopsy), regarding my final decision. Prior to the the final decision I studied extensively on all my treatment options.
I soon received the first of three hormone injections over a three month period. Preparations for the actual surgery got underway in the latter part of June. I went under the "ice" about 7:30am Friday, July 5, 1998, and some 30 hours later my wife took me hone. Two days later I was up and about and able to take a walk around the block. Subsequently more tests followed including a MRI to check on any scar tissue.
Now for the good news. Three months after surgery a PSA test revealed a reading of 0.2 and this number has been constant for the past eight years.
I am a very lucky man on three counts: one, may family physician recognized some was amiss and did something; two: the cryosurgery was successful thanks to Dr. Donnelly and his co-workers; and three, my wife stood by me and put up with me during trying times.
What to do next? The doctor explained that there was no hurray, that I would not die because of the "showing". Although my PSA was 7.5 the Gleason score was 2/4 (6). My wife and I decided right there and then I would undergo therapy of some kin. Dr. Donnelly then mentioned he was starting a clinical test program to test the efficacy of cryosurgery, but before any action along this line is undertaken, a series of test would have to be held. After these tests had been completed I was told I was an "excellent candidate" for cryosurgery.
No long after I was contacted by Cheryl Scott RN, the coordinator of the program (incidentally, Cheryl was the one earlier who appraised me of the results of the biopsy), regarding my final decision. Prior to the the final decision I studied extensively on all my treatment options.
I soon received the first of three hormone injections over a three month period. Preparations for the actual surgery got underway in the latter part of June. I went under the "ice" about 7:30am Friday, July 5, 1998, and some 30 hours later my wife took me hone. Two days later I was up and about and able to take a walk around the block. Subsequently more tests followed including a MRI to check on any scar tissue.
Now for the good news. Three months after surgery a PSA test revealed a reading of 0.2 and this number has been constant for the past eight years.
I am a very lucky man on three counts: one, may family physician recognized some was amiss and did something; two: the cryosurgery was successful thanks to Dr. Donnelly and his co-workers; and three, my wife stood by me and put up with me during trying times.

Alan Rankin
It was after my annual medical at age 58 I received a call from my doctor. The digital exam showed the prostate gland was enlarged but smooth and soft. The result of the PSA came back 7. My doctor was concerned and sent me to an urologist, which took about four months waiting time. In his office a large poster displayed an elderly man standing in front of a urinal, a young boy was standing behind him with legs crossed. The caption was "Never line up behind a grey haired man if you have to go real bad." I knew I was in the right place. I was sent for my first biopsy not knowing what to expect, but thinking the worst. The urologist did not take the time to explain the procedure of the biopsy. I arrived at the Prostate Cancer Clinic with my wife and a "full bladder". The thought of Cancer was on my mind even though I told my family I was not worried. The nurse asked me to undress down to my socks and shorts, and put on the house- coat that is always wide open at the back. The ultra sound was completed and off to the bathroom to empty my bladder. I went back into the little change room and waited for the unexpected. Dr. Wiseman told me they would be taking 10 samples and asked me to lie down on the examining bed and face the wall. My shorts were pulled down and something that felt the size of a roto-rooter got my attention. There was no local anesthetic offered at that time. The first five pieces of flesh were not that bad, but I started the count down for the last five. At the end of the biopsy, I walked out and was able to have a smile on my face.
The results came back negative and I was told it would be a waiting and watching for any changes. I had four biopsies over an eight year period. My PSA went up every two years, from 7, 11, and 17 to 26. It was the last biopsy that showed there was cancer in one of the lobes of the prostate gland. My Gleason count was 8. On my second visit for a biopsy, I was lying on the exam table, face to the wall, and Dr. Wiseman said he thought he recognized me. I said I hope it was not from the end he was viewing. He said no, I saw your face when you came in. There are over one million hits on the internet for prostate cancer. I have looked at a lot of them. One of the articles I read stated if one hundred men were diagnosed with prostate cancer, and they did nothing for prevention, eighty would die with prostate cancer and twenty would die because of it. I told this to my urologist Dr. Metcalfe, he said unfortunately you are in the twenty men that would die without treatment. With a PSA of 26 and a Gleason of 8, my options for treatment were limited. The two options that were recommended to me was surgery or radiation. It was decision time.
The two options that were recommended are the ones I least wanted. I preferred the radiation seed implants referred to as Brachy Therapy or the freezing referred to as Cryo Therapy. After looking at radiation and surgery, I elected for surgery because I was told it was very difficult to do surgery after radiation as the prostate gland turns into scar tissue.
Radical Prostatectomy:
After checking into the Rocky View Hospital, I was led to a change room and told to put on a "back end open" housecoat. They put me in a reclining chair with warm blankets and asked me to wait. At the appropriate time I was led down a long corridor into the operating room. Dr. Metcalfe said if I wanted to bolt, now was the time. I smiled and climbed up on the table. I was told to sit up, bend over, bend my knees and grab my legs. That's the last thing I remember until a nurse asked me if I could move my toes. They placed me on the hospital bed with I Vs in my arm and the unforgettable catheter plugged in for hands free use. The scrub nurse came and said she had to wash me. I said I had a shower this morning so it was not necessary. She used a damp cloth and wiped my leg, it was a bright orange colour. She then lifted up the blankets and my fancy nightshirt and proceeded to scrub the disinfectant off my shy body. Two months later I arrived at the hospital to visit a friend that had the same surgery. The same nurse was about to scrub him down. I told her she had done the same thing to me earlier. She quickly replied in her Scottish accent that she did not recognize me with me clothes on.
The treatment the nurses and staff gave at the Rocky View was first class. The one thing that surprised me, there was NO PAIN from the operation. My throat was a little sore from the tube they inserted during the operation. Every time the nurses came to the room they asked if I had passed gas. They said this was the only section of the hospital they cheered when a patient passed gas. I got my cheer on the second day! My grand daughter was born in the same hospital while I was recovering. I went down to see her for the first time pushing the IV and catheter holder and wearing a new housecoat. I had my picture taken holding the precious bundle. She will wonder in years to come why grandpa had his housecoat on. The two concerns I had were incontinence and erectile dysfunction. They gave us an exercise for the first problem. I can proudly say I have control of my bladder. The second problem, we started working on "it", but it has been interrupted by Hormone Therapy. On the tenth day after surgery I went to Dr. Metcalfe's office to have the catheter removed. He had a very young female urologist observing him with patients. He asked me to lie on the table and he would remove the tube on the count of three. This should have been a warning. It felt like the tube was attached to my knee. It was about two months after surgery I was able to go golfing. I enjoyed the game even with the high score.
Three months following surgery my PSA was virtually non-detectable 0.01. The doctor said they did biopsies on the surrounding lymph nodes and the results were negative. What a relief, I thought we had beaten the big "C". I was sent for PSA testing every three months for the next year. The results were very low 0.1 and 0.3 and the fourth test showed 0.4. No big deal I thought! Dr. Metcalfe said the PSA should not be rising with the prostate removed. He referred me back to Dr. Husain at the Tom Baker Center. It was recommended that I consider Hormone Therapy and I volunteered for a case study. They randomly selected the patients for a six-month or a two-year study. I was selected for the two-year study and told how lucky I was. At the same time I signed up for a study with the University of Calgary about physical activity of cancer patients on Hormone Therapy. The best part of the Hormone injection is the fuel cost we have saved over this past winter. I never knew what a "Hot Flush" was before. Just ask me now. The size of the needle they use to inject the time release tablet seems larger then the big knitting needles. I was told each injection was worth $1,400.00 and paid for by the Cancer Clinic. Being in two case studies has given more attention to my problem then just a patient to a doctor. I should have the final results from the U of C study by September showing how I ranked with the other old farts during the physical activities.
External Beam Radiation:
Three months after Hormone Therapy, they scheduled me for radiation. They did an ultra sound and placed three little tattoos on my body for the laser beam on the radiation machine to lock onto. I was told 25% of the patients have no problems with side effects, 50% have a few side effects and the other 25% have several problems. Thirty-nine treatments were scheduled for every morning except Saturday and Sunday. The procedure was fast and very simple. A friend at the gym where I have a workout each week day morning asked me what they do. I said you go into the radiation room with two or three young ladies and they ask you to take your pants off and get on the bed. He replied, "It could only happen in America". Each treatment took about ten minutes from the time you went into the room until you were walking outside. Side effects were minimal. My bowls became very active with an abundance of gas. I had the urge to go to the bathroom, mostly gas but sometimes there was the one percent substance. You did not want to take a chance on any surprises so you always sat down to do the job.
The last two weeks of treatment, I began to get tired in the afternoons. A fifteen-minute power nap was all that I needed. I asked the girls if they knew how the treatments were going and if they were doing any good. I was told they did not know and would only find out when treatments were complete and the results were checked. My last PSA showed 0.02 and I was told to come back in six months. I requested the Hormone injections stop after one year because the flushes were very intense and woke me up six to seven times each night. January was my last injection and I was told it would take until November for the estrogen to dissipate from my body. When the hormones and testosterone are back to normal, I will then start working on problem # 2. I feel very pleased with the treatment I have received from all departments that treat cancer. Not once did I feel I was getting second-class treatment. My sons wanted me to go to the Mayo Clinic in Arizona. We arranged an appointment but I ended up staying in Calgary because I truly feel we have world-class facilities for cancer treatment in our own back yard.
Volunteering at the Prostate Cancer Clinic:
I felt I had to give something back because of the treatment I had received. I now volunteer each Tuesday morning from 8:30 until noon. I talk with the patients that come in for a biopsy. Some of these men are very nervous and have only a vague idea of what is taking place. Men in general, do not like to talk about things that affect their "Man-hood". It gives me great pleasure talking with these men and their wives and answering questions they felt uncomfortable asking. I always start the conversation by telling them I am a volunteer and I have had four biopsies in the past. All without a local anesthetic! I can't give you advice, but I can tell you my experiences. I invite them to come to the resource center to ask questions and check out books. I tell them the more information you have, the easier it will be to make a decision about treatment if it is required. I wish them good luck and tell them it will most likely be a "Watch and Wait" situation.
The results came back negative and I was told it would be a waiting and watching for any changes. I had four biopsies over an eight year period. My PSA went up every two years, from 7, 11, and 17 to 26. It was the last biopsy that showed there was cancer in one of the lobes of the prostate gland. My Gleason count was 8. On my second visit for a biopsy, I was lying on the exam table, face to the wall, and Dr. Wiseman said he thought he recognized me. I said I hope it was not from the end he was viewing. He said no, I saw your face when you came in. There are over one million hits on the internet for prostate cancer. I have looked at a lot of them. One of the articles I read stated if one hundred men were diagnosed with prostate cancer, and they did nothing for prevention, eighty would die with prostate cancer and twenty would die because of it. I told this to my urologist Dr. Metcalfe, he said unfortunately you are in the twenty men that would die without treatment. With a PSA of 26 and a Gleason of 8, my options for treatment were limited. The two options that were recommended to me was surgery or radiation. It was decision time.
The two options that were recommended are the ones I least wanted. I preferred the radiation seed implants referred to as Brachy Therapy or the freezing referred to as Cryo Therapy. After looking at radiation and surgery, I elected for surgery because I was told it was very difficult to do surgery after radiation as the prostate gland turns into scar tissue.
Radical Prostatectomy:
After checking into the Rocky View Hospital, I was led to a change room and told to put on a "back end open" housecoat. They put me in a reclining chair with warm blankets and asked me to wait. At the appropriate time I was led down a long corridor into the operating room. Dr. Metcalfe said if I wanted to bolt, now was the time. I smiled and climbed up on the table. I was told to sit up, bend over, bend my knees and grab my legs. That's the last thing I remember until a nurse asked me if I could move my toes. They placed me on the hospital bed with I Vs in my arm and the unforgettable catheter plugged in for hands free use. The scrub nurse came and said she had to wash me. I said I had a shower this morning so it was not necessary. She used a damp cloth and wiped my leg, it was a bright orange colour. She then lifted up the blankets and my fancy nightshirt and proceeded to scrub the disinfectant off my shy body. Two months later I arrived at the hospital to visit a friend that had the same surgery. The same nurse was about to scrub him down. I told her she had done the same thing to me earlier. She quickly replied in her Scottish accent that she did not recognize me with me clothes on.
The treatment the nurses and staff gave at the Rocky View was first class. The one thing that surprised me, there was NO PAIN from the operation. My throat was a little sore from the tube they inserted during the operation. Every time the nurses came to the room they asked if I had passed gas. They said this was the only section of the hospital they cheered when a patient passed gas. I got my cheer on the second day! My grand daughter was born in the same hospital while I was recovering. I went down to see her for the first time pushing the IV and catheter holder and wearing a new housecoat. I had my picture taken holding the precious bundle. She will wonder in years to come why grandpa had his housecoat on. The two concerns I had were incontinence and erectile dysfunction. They gave us an exercise for the first problem. I can proudly say I have control of my bladder. The second problem, we started working on "it", but it has been interrupted by Hormone Therapy. On the tenth day after surgery I went to Dr. Metcalfe's office to have the catheter removed. He had a very young female urologist observing him with patients. He asked me to lie on the table and he would remove the tube on the count of three. This should have been a warning. It felt like the tube was attached to my knee. It was about two months after surgery I was able to go golfing. I enjoyed the game even with the high score.
Three months following surgery my PSA was virtually non-detectable 0.01. The doctor said they did biopsies on the surrounding lymph nodes and the results were negative. What a relief, I thought we had beaten the big "C". I was sent for PSA testing every three months for the next year. The results were very low 0.1 and 0.3 and the fourth test showed 0.4. No big deal I thought! Dr. Metcalfe said the PSA should not be rising with the prostate removed. He referred me back to Dr. Husain at the Tom Baker Center. It was recommended that I consider Hormone Therapy and I volunteered for a case study. They randomly selected the patients for a six-month or a two-year study. I was selected for the two-year study and told how lucky I was. At the same time I signed up for a study with the University of Calgary about physical activity of cancer patients on Hormone Therapy. The best part of the Hormone injection is the fuel cost we have saved over this past winter. I never knew what a "Hot Flush" was before. Just ask me now. The size of the needle they use to inject the time release tablet seems larger then the big knitting needles. I was told each injection was worth $1,400.00 and paid for by the Cancer Clinic. Being in two case studies has given more attention to my problem then just a patient to a doctor. I should have the final results from the U of C study by September showing how I ranked with the other old farts during the physical activities.
External Beam Radiation:
Three months after Hormone Therapy, they scheduled me for radiation. They did an ultra sound and placed three little tattoos on my body for the laser beam on the radiation machine to lock onto. I was told 25% of the patients have no problems with side effects, 50% have a few side effects and the other 25% have several problems. Thirty-nine treatments were scheduled for every morning except Saturday and Sunday. The procedure was fast and very simple. A friend at the gym where I have a workout each week day morning asked me what they do. I said you go into the radiation room with two or three young ladies and they ask you to take your pants off and get on the bed. He replied, "It could only happen in America". Each treatment took about ten minutes from the time you went into the room until you were walking outside. Side effects were minimal. My bowls became very active with an abundance of gas. I had the urge to go to the bathroom, mostly gas but sometimes there was the one percent substance. You did not want to take a chance on any surprises so you always sat down to do the job.
The last two weeks of treatment, I began to get tired in the afternoons. A fifteen-minute power nap was all that I needed. I asked the girls if they knew how the treatments were going and if they were doing any good. I was told they did not know and would only find out when treatments were complete and the results were checked. My last PSA showed 0.02 and I was told to come back in six months. I requested the Hormone injections stop after one year because the flushes were very intense and woke me up six to seven times each night. January was my last injection and I was told it would take until November for the estrogen to dissipate from my body. When the hormones and testosterone are back to normal, I will then start working on problem # 2. I feel very pleased with the treatment I have received from all departments that treat cancer. Not once did I feel I was getting second-class treatment. My sons wanted me to go to the Mayo Clinic in Arizona. We arranged an appointment but I ended up staying in Calgary because I truly feel we have world-class facilities for cancer treatment in our own back yard.
Volunteering at the Prostate Cancer Clinic:
I felt I had to give something back because of the treatment I had received. I now volunteer each Tuesday morning from 8:30 until noon. I talk with the patients that come in for a biopsy. Some of these men are very nervous and have only a vague idea of what is taking place. Men in general, do not like to talk about things that affect their "Man-hood". It gives me great pleasure talking with these men and their wives and answering questions they felt uncomfortable asking. I always start the conversation by telling them I am a volunteer and I have had four biopsies in the past. All without a local anesthetic! I can't give you advice, but I can tell you my experiences. I invite them to come to the resource center to ask questions and check out books. I tell them the more information you have, the easier it will be to make a decision about treatment if it is required. I wish them good luck and tell them it will most likely be a "Watch and Wait" situation.

Gil Carson
Cancer Survivor, Age 68
Description
Name
Designation
Description
Name
Designation
Description
Name
Designation
-
Timeline Title 1
Click here to change text
-
rereser
esrrrr
-
355335
35
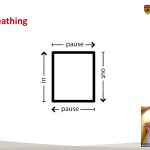 Mindfulness for Managing Cancer-related StressClinical psychologist Dr. Linda E. Carlson joins us to discuss how to train your mind to deal with the stress that comes with a cancer diagnosis along with providing breathing exercises to help regulate your body systems and cope with everyday stressors. […]
Mindfulness for Managing Cancer-related StressClinical psychologist Dr. Linda E. Carlson joins us to discuss how to train your mind to deal with the stress that comes with a cancer diagnosis along with providing breathing exercises to help regulate your body systems and cope with everyday stressors. […] Navigating Sexual Relationships After CancerRegistered Provisional Psychologist Chelsea Anderson joins us from Walker Psychological to talk about biopsychosocial models for restoring intimacy after prostate cancer. She also discusses erectile treatments, and strategies for communication between partners. […]
Navigating Sexual Relationships After CancerRegistered Provisional Psychologist Chelsea Anderson joins us from Walker Psychological to talk about biopsychosocial models for restoring intimacy after prostate cancer. She also discusses erectile treatments, and strategies for communication between partners. […] Miracle Home CareFeven Gebregiorgis joins us to discuss Miracle Home Care, a Calgary-based home care provider. She discusses why one might need home care, whether it's to help administer medications, help with routine care, or respite for those caring for someone with extra needs. […]
Miracle Home CareFeven Gebregiorgis joins us to discuss Miracle Home Care, a Calgary-based home care provider. She discusses why one might need home care, whether it's to help administer medications, help with routine care, or respite for those caring for someone with extra needs. […] Wellspring – No One Has to Face Cancer AloneScott Patterson, centre manager for Carma House, joins us to talk about Wellspring Alberta, its history, how it has evolved over the years to reach people across Alberta and the litany of services and supports it offers those dealing with cancer. […]
Wellspring – No One Has to Face Cancer AloneScott Patterson, centre manager for Carma House, joins us to talk about Wellspring Alberta, its history, how it has evolved over the years to reach people across Alberta and the litany of services and supports it offers those dealing with cancer. […] “Now What?” – Living with Prostate Cancer and ThrivingCounselling Therapist Jeremiah La Follette joins us for a motivational talk about how to turn the anticipatory grief of a prostate cancer diagnosis into a source of strength and power by using pragmatic thinking and step by step action - to thrive beyond diagnosis as a warrior. […]
“Now What?” – Living with Prostate Cancer and ThrivingCounselling Therapist Jeremiah La Follette joins us for a motivational talk about how to turn the anticipatory grief of a prostate cancer diagnosis into a source of strength and power by using pragmatic thinking and step by step action - to thrive beyond diagnosis as a warrior. […]
this is a hero
John De Hart

